
Ready, Set, TEAM: Prepare Your Hospital for Mandatory Surgical Episode Payments
By Georgia Green
Senior Manager
Health Care Consulting Practice, Moss Adams
Original Publish Date: December 3, 2024
The transition to value-based care took another big step forward with the introduction of the Transforming Episode Accountability Model (TEAM Model), finalized in the 2025 Inpatient Prospective Payment System (IPPS) Rule.
Per the Centers for Medicare & Medicaid Services (CMS), this mandatory payment model puts the financial responsibility for the cost of a patient’s care for a predetermined period of time on hospitals and aims to enhance accountability and improve patient outcomes in acute care hospitals across the United States.
Overview of the TEAM Model
Beginning January 1, 2026, this five-year initiative targets Medicare fee-for-service patients, focusing on reducing cost to CMS while theoretically improving quality and outcomes for patients undergoing five types of surgeries.
CMS indicates the model specifically addresses fragmentation in care for patients undergoing these surgical procedures and aims to decrease readmissions and improve care transitions for these patients.
Under the model, selected hospitals become financially responsible for the total cost of the patient’s care during the hospital anchor stay or outpatient procedure and 30 days post-discharge.
Key Features of the TEAM Model
Key features of the model are as follows.
Mandatory Participation
The TEAM Model will be implemented at 741 acute care hospitals located in 188 randomly selected Core Based Statistical Areas (CBSAs) throughout the nation, roughly 23% of all CBSAs. Hospitals paid under the IPPS and located in these CBSAs are required to participate in the TEAM Model.
Voluntary Participation
Hospitals participating in the Bundled Payments for Care Improvement Advanced (BPCI-A) or Comprehensive Care for Joint Replacement (CJR) models may voluntarily opt in, regardless of location. To do so, they must submit a participation letter to CMS in January 2025. Additional details are forthcoming.
Surgery Types
The following surgeries are included in the TEAM Model because they are high volume, high-cost procedures:
- Lower extremity joint replacement (LEJR)
- Surgical hip femur fracture treatment (SHFFT)
- Spinal fusion
- Coronary artery bypass graft (CABG)
- Major bowel procedure
The model includes both elective and emergent procedures.
Episode Total Cost of Care
The model accounts for the total Medicare Parts A and B cost of care during the initial hospital visit or procedure for outpatient episodes, plus all expenditures incurred within 30 days post-discharge. This includes all sites of care and types of expenditures, including:
- Inpatient hospital readmission
- Skilled nursing facility (SNF)
- Inpatient rehabilitation facility (IRF)
- Home health agency (HHA)
- Hospice
- Hospital outpatient services
- Physician services
- Part B pharmaceuticals
- Clinical lab services
- Durable medical equipment (DME)
Episodes may be associated with multiple hospitalizations through readmissions or transfers. When more than one hospitalization occurs during an episode, CMS will hold the hospital to which the episode is initiated accountable. Costs for services extending beyond the episode period will be prorated.
There’s no change to billing and revenue cycle practices for the selected hospitals or other care providers, as the model financial reconciliation calculation is performed by CMS retrospectively.
That said, organizations should absolutely be analyzing potential impact and planning to mitigate what are sure to be financial and coordination of care challenges.
Exclusions
Like other value-based models, CMS acknowledges there are extraordinary cases that should be excluded from the financial reconciliation. Considering that, truncation is set at the 99th percentile, meaning the top 1% most expensive episodes by Medicare Severity-Diagnosis Related Group (MS-DRG), by region, will be carved out.
Exclusions will be minimal and consistent with prior models BPCI-A and CJR. Costs not included in the TEAM Model episode include:
- Hospital admissions and readmissions for specific categories of diagnoses, such as oncology, trauma medical admissions, organ transplant, and ventricular shunts determined by MS–DRGs
- Excluded Major Diagnostic Categories (MDC), such as MDC 02 Diseases and Disorders of the Eye; MDC 14 Pregnancy, Childbirth, and Puerperium; MDC 15 Newborns and Other Neonates with Conditions Originating in Perinatal Period; and MDC 25 Human immunodeficiency virus infections
- IPPS new technology add-on payments for drugs, technologies, and services, billed using CMS value code 77
- Hospital Outpatient Prospective Payment System (OPPS) transitional pass-through payments for medical devices
- Hemophilia clotting factor drugs
- Other high cost, low volume drugs or biologicals
Target Pricing
CMS will set an annual target price for each surgery type, encompassing both the anchor procedure and the 30-day post-discharge period.
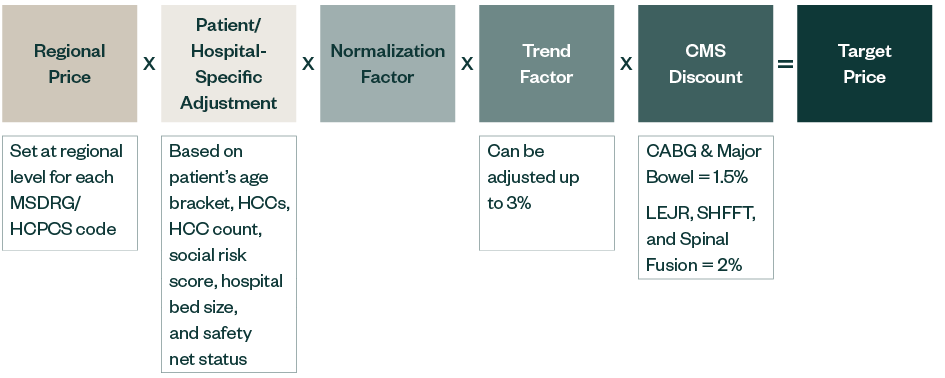
The target price is a product of the regional price, patient- and hospital-specific adjustments, normalization factors, trend factor capped at 3%, and a CMS discount factor—1.5% for CABG and major bowel procedure and 2% for LEJR, SHFFT, and spinal fusion. The full details of target price calculation will be included in forthcoming guidance from CMS.
The regions for the TEAM Model are defined as the nine US census divisions.
Model Payments
The Net Payment Reconciliation Amount (NPRA) is calculated as target price minus actual spend.
Payments will be reconciled annually, approximately six months after the end of each performance year. The payment or recoupment amount will include adjustments based on quality performance, ensuring financial incentives align with the quality of care delivered.
Risk and Reward Tracks
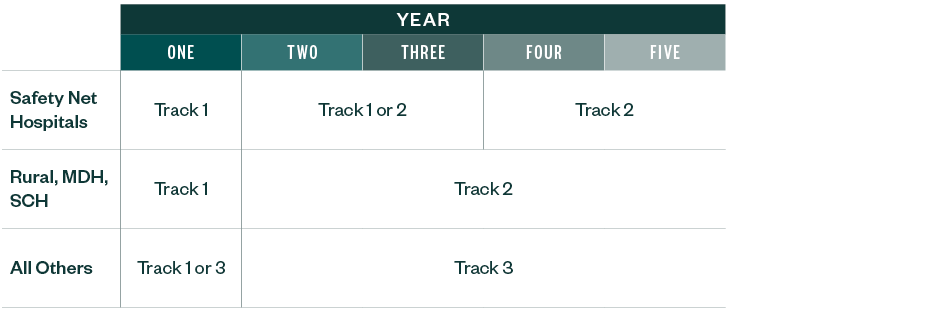
The TEAM Model introduces three tracks, each with varying levels of risk and reward.
- Track 1: No downside risk, low reward potential with a 10% stop-gain limit. Quality adjustments can increase payments by up to +10%.
- Track 2: Low risk and reward, featuring a 5% stop-loss and stop-gain limit. Quality adjustments can vary from +10% to -15%.
- Track 3: High risk and reward, with a 20% stop-loss and stop-gain limit. Quality adjustments can range from +10% to -10%.
The hospital type determines eligibility for each track. CMS is allowing safety net hospitals, rural, Medicare dependent hospitals (MDH), and sole community hospitals (SCH) to stay at the low-risk track for the length of the model. Participants have the option to opt into a higher-risk track.
Hospitals in Tracks 2 and 3 potentially qualify for Advanced Alternative Payment Model (APM) status if they utilize certified electronic health record technology (CEHRT), which may increase Medicare Part B reimbursement under the Quality Payment Program.
Quality Measures
The financial performance of participants will be influenced by a composite quality score, derived from several key metrics:
- Hybrid Hospital-Wide All-Cause Readmission Measure. PY1 measurement period: July 1, 2024, to June 30, 2025.
- CMS Patient Safety Indicator (PSI-90). PY1 measurement period: July 1, 2023, to June 30, 2025.
- Patient Reported Outcome-Based Performance Measure (PRO-PM) for LEJR. PY1 measurement period: July 1, 2024, to June 30, 2025.
- Hospital Harm and Failure to Rescue Measures. Start in performance year two.
Hospitals’ performance scores will be publicly reported by CMS on their website, after reporting to participants. Hospitals should be aware that the data measurement periods are already underway for performance year one.
Model Requirements
To ensure effective implementation, the TEAM Model includes specific requirements:
- Beneficiary Notification: Hospitals must provide written letters to attributed beneficiaries using a CMS template, ensuring transparency and communication.
- Referral to Primary Care Provider (PCP): A referral to a PCP is required prior to discharge for all beneficiaries, promoting continuity of care and successful care transitions.
- Health-Related Social Needs (HRSN) Screening: Beneficiaries must be screened for at least four of five HRSN domains, as defined by the Hospital Inpatient Quality Reporting (IQR) Program measures SDOH-1 and SDOH-2, helping hospitals understand and support social determinants that can affect health outcomes.
- PRO-PM for LEJR Reporting: Pre- and post-operative surveys will be sent to patients, capturing their experiences and outcomes.
Voluntary Reporting
CMS encourages hospitals to report these voluntary items to improve understanding of health disparities and enhance the quality of care provided to diverse patient populations.
Health Equity Plan
Hospitals can create a health equity plan to identify disparities, set goals, develop intervention strategies, and establish performance measures to promote health equity.
HRSN Screening Positivity Data
Hospitals can report aggregated data results including positivity rates from HRSN screenings to CMS. Hospitals that report this data may also report information about their HRSN screening policies and procedures.
Demographic Data
Hospitals can collect and report beneficiary-level demographic data to CMS, which may include:
- Race
- Ethnicity
- Language
- Disability
- Sexual orientation
- Gender identity
Benefits
The TEAM Model offers several advantages for patients and participating hospitals.
Patient Experience
The model aims to reduce readmissions and promote coordinated care, enhancing the overall patient experience.
Potential Earnings
Hospitals can benefit from reconciliation payments based on their performance in managing care episodes.
Model Overlap
Patients may be included in both the TEAM Model and Accountable Care Organizations (ACOs) without any payment adjustments, allowing for a more integrated approach to care. This is also a dual financial benefit opportunity for hospitals that are in both programs.
Incentive Sharing
Participants in the TEAM Model will have the opportunity to share payments with physicians and other providers involved in the surgical episode, fostering collaboration and enhancing care delivery across the network.
Access to Claims Data
Participants will gain access to valuable claims data, aiding in performance evaluation and improvement and increasing understanding of care patterns and network leakage.
Engagement Mechanism
The model provides a framework to engage specialists and service lines in care transformation, fostering collaboration amongst hospital and post-acute providers.
Future Readiness
Hospitals will be well-positioned for success if CMS makes episode-based payments mandatory in the future.
Alignment with Other Value-Based Payment Arrangements
The model allows for operational alignment with other value-based payment arrangements, such as the Medicare Shared Savings Program (MSSP) or commercial payor contracts of a similar nature.
Leverage CMS Waivers
Participants may leverage CMS waivers and flexibilities, such as the SNF Three-Day Rule Waiver, to enhance care delivery.
How to Prepare
Participants in Tracks 2 and 3 face downside risk in the model, as they will owe a recoupment payment to CMS if the target price is not achieved. The episode target prices are achievable but will require a concerted effort by hospital leaders to develop a strategy, implement operational tactics, monitor performance, and provide ongoing feedback to stakeholders. To effectively prepare for the TEAM Model, hospitals should consider the following steps.
Confirm Participation
Verify your hospital's participation through CMS’s published list.
Identify CMS Points of Contact
Complete and submit the Primary Point of Contact Identification Form to CMS to identify individuals that will receive communications.
Identify Stakeholders and Form a Workgroup
Assemble a team that includes stakeholders from clinical and surgery service lines, finance, quality, analytics, care management, and value-based care.
Benchmark Your Performance
It’s helpful to understand how you stack up against the rest of the country, and particularly, your region, since target prices are set at a regional level.
If you have access to claims data, such as CMS shadow bundle data, or another data source, you can compare your hospital’s episodic costs to regional and national benchmarks for each surgery type.
By comparing outcomes for urgent versus elective procedures, the hospital may identify if there’s a large differential and take steps to manage the urgent cases more deliberately. Additionally, hospitals can assess current quality score performance on the required measures to identify opportunities for improvement.
Participants may also want to examine process measures, such as the rate of PCP and transitional care management (TCM) visits within 14 days post-discharge. Although this isn’t specifically graded in the model, doing well on these measures will help achieve the model goals.
Begin Operational Planning
The TEAM Model requires engagement from multiple hospital leaders to develop and deploy strategies that will improve operations and achieve the model’s goals. Strategies to consider include:
- Develop or expand care transition, care coordination, and care planning capacity. These are Medicare-billable services and can provide an enhanced revenue stream.
- Increase provider education and collaboration among surgical specialists, primary care, and therapists. Everybody on the surgical patients’ care team should understand that the hospital is participating in the model, and the potential consequences and benefits.
- Understand and prepare to report the model’s quality measures. Provide staff education, as needed.
- Optimize Hierarchical Condition Category (HCC) coding practices to ensure CMS is setting an accurate target price.
Consider Clinical Transformation and Service Line Optimization
While the items above may represent the nuts and bolts for succeeding in the TEAM Model, it’s critical to keep the big picture in mind: the TEAM Model can be a mechanism and a motivation moving your hospital toward clinical transformation. These big picture goals include:
- Improve your key service lines by developing sophisticated management and coordination structures and processes to drive efficiency and quality.
- Enhance pre- and post-operative planning and workflows to improve communication amongst the patient and care team, and provide a consistent, replicable experience using best practices which may include Lean or Six Sigma principles.
- Reduce care variation.
- Decrease length of stay.
- Increase efficiency.
Take a Data-Driven Approach
Participating in the TEAM Model will provide complete claims data about the episodes for which you are accountable, meaning you can see all Medicare claims at all sites of care, updated on a monthly basis. Additionally, CMS typically provides summarized performance information on a quarterly and annual basis. Hospitals should plan to ingest and understand this data.
- Develop the capacity and workflow to receive and analyze claims and utilization data from CMS.
- Use the data to identify both high- and low-performers within your network and provide targeted education.
- Use the data to identify high-value post-acute care partners.
- Create internal reporting mechanisms for ongoing performance monitoring, ensuring transparency, and incentivizing physicians.
Join the Moss Adams TEAM Model Peer Group
We hope you’ll consider joining the Moss Adams TEAM Model Peer Group for additional support and resources.
You’ll be able to connect with other hospital leaders who are navigating the same challenges and collaborate on solutions.
We’re Here to Help
The complexity of the TEAM Model may be a significant challenge to hospitals—even those that have well-established care management programs and are familiar with value-based payments. For those that are new to risk, this model’s requirements may be daunting. The good news is the same efforts and strategies that drive overall success in health care systems will help here. Please reach out to your Moss Adams professional if you would like to join the peer group, or want assistance with:
- Understanding how the TEAM Model works
- Benchmarking your performance
- Financial projections
- Operational planning and execution
- Quality reporting and improvement
- Strategic network development
- Data and performance analytics
- Provider and staff education
- Development of a health equity plan
- Any other questions or needs that may arise
Additional Resources